RWE4Decisions is a multi-stakeholder Learning Network on how fit-for-purpose RWE over the life cycle of highly innovative medicines can inform HTA/Payer decisions.
Improving Rare Disease Data Availability and Quality for HTA/Payers

RWE4Decisions Symposium: Mobilising Real-World Data to Enhance HTA/Payer Decision-Making

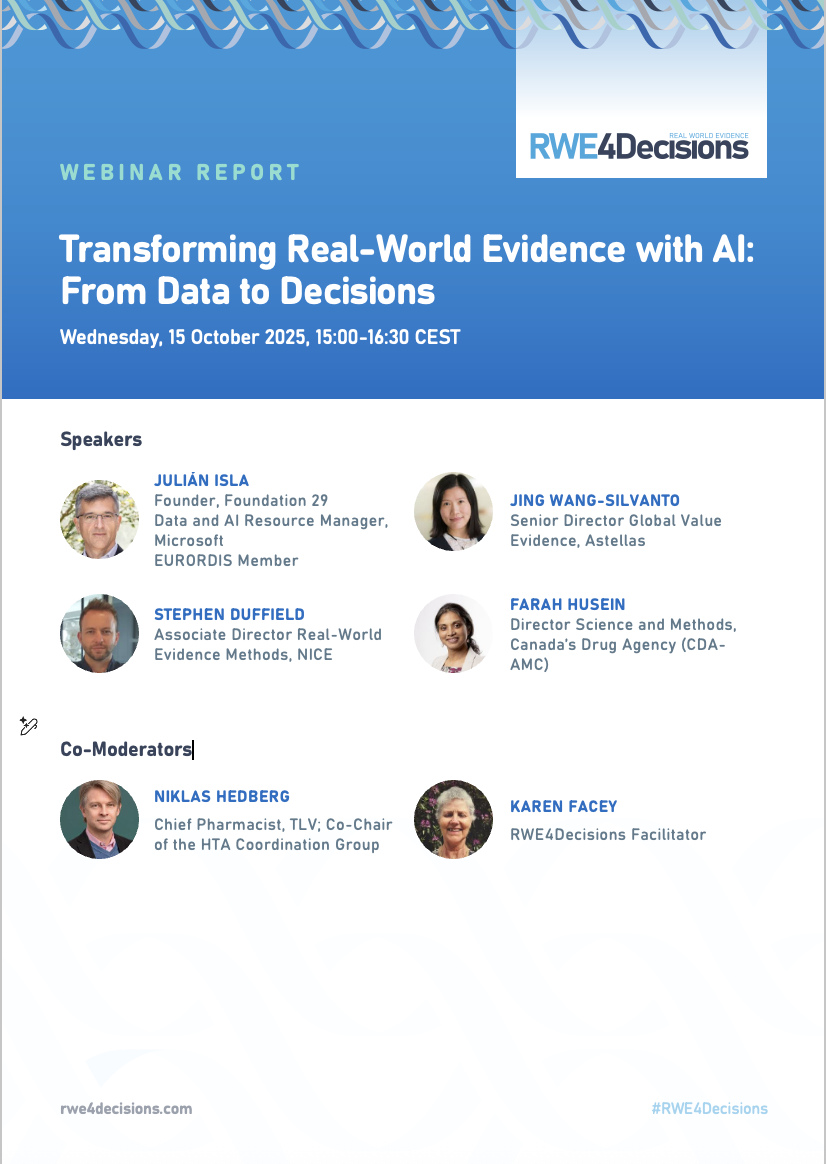
Public Webinar: Transforming Real-World Evidence with AI: From Data to Decisions
Public Webinar: From Policy to Practice: EHDS Implementation to Support Better Real-World Evidence for HTA/Payers



























Explore our latest resources designed to support real-world evidence planning and evaluation:
March 24, 2025
Report

September 12, 2024
Report

November 27, 2022
Press release

June 17, 2025
Paper

February 17, 2025

November 2, 2022
Paper

September 27, 2020
Paper

December 3, 2025
August 27, 2025
Call to action

March 5, 2025
Policy brief
February 3, 2026
Report

May 22, 2025
Report

January 23, 2025